Introduction to Reimbursable Prevention Apps
DiGAs are not the only type of application that can be reimbursed by statutory insurers. The Digital Prevention Course Framework provides another business case.
Digital health products usually try to provide an alternative cure. The diagnosis is already made, the patient is sick. They need a resolution. The whole German healthcare system is build this way, it is not the fault of digital mental health operators. Most healthcare systems are. The problem: fixing issues is expensive. The remedy: preventing risk factors from turning into diagnoses.
Whilst DiGAs get all the buzz in the mental health community, there is another type of insurance-financed business model I hear people talk about rarely: prevention apps. Whilst reimbursements are lower per user, these don't require a prescription and have lower regulatory burdens. (You still need to prove efficacy in studies, though!)
So here is a quick overview of the digital prevention framework. Maybe it will spark a new idea or two:
What is digital prevention?
Digital prevention can come in many forms. The GKV Spitzenverband, the umbrella organization for all statutory German health insurers, provides the following structure:
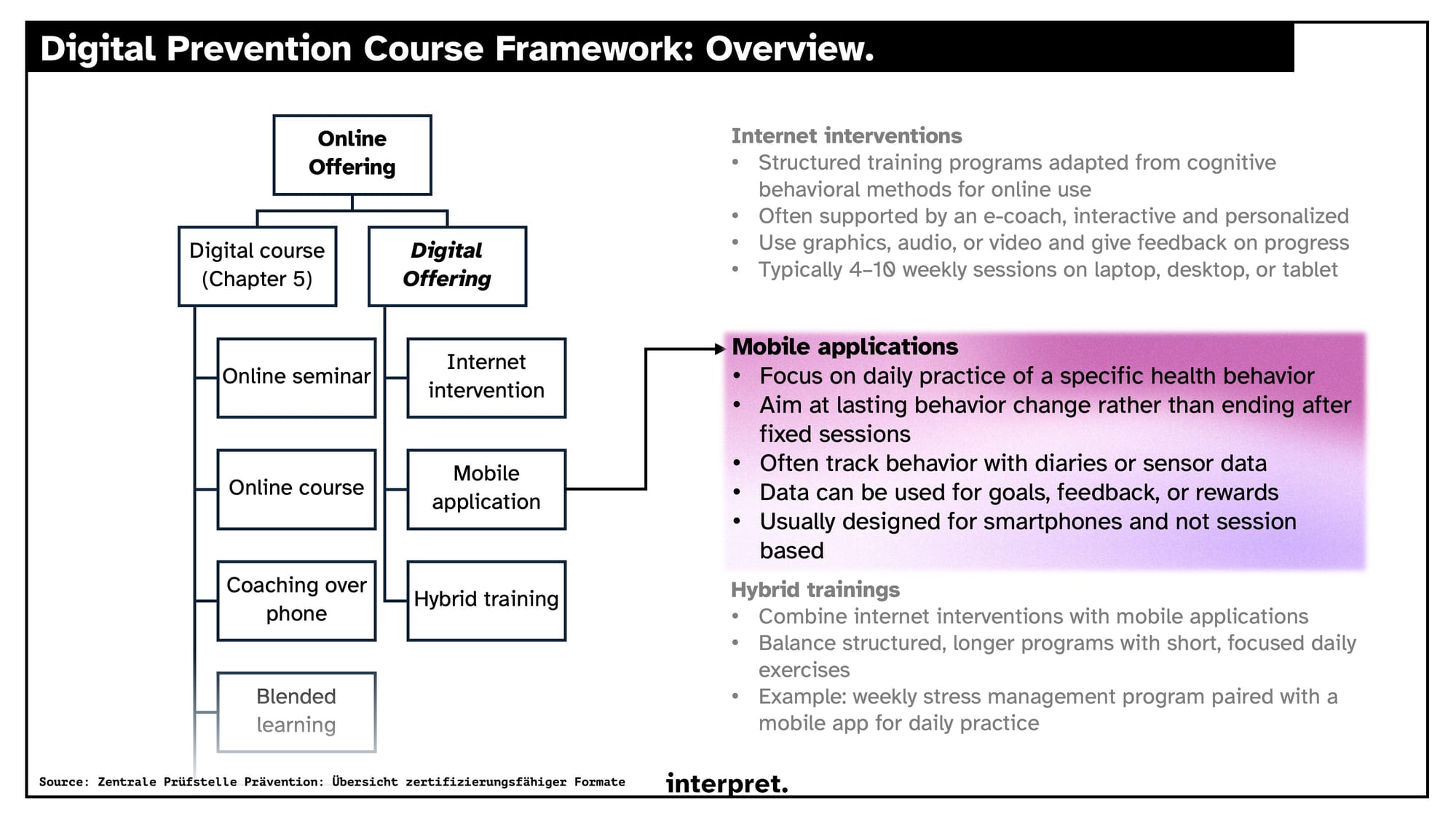
These mobile applications are laid out in chapter 7 of the Guidance on Prevention by the GKV. Since Juli 2021, this guidance is set to include digital prevention as a service insurers need to cover. In 2023, chapter 7 was added to clarify the resulting prevention course apps. The general idea. Educated people and help them learn new skills to lead a healthier life and be less expensive as members.
The GKV specifies 4 areas of prevention, in which products can be certified for insurance coverage:
- movement habits: reduction of personal health risks through pointed sports activities, general increase in physical activity
- nutrition: reduction of overweight, prevention of malnutrition
- stress- and resource management: learning of stress management skills, learning relaxation techniques
- consumption of addictive substances: support of non-smoking, more responsible alcohol consumption
Gym memberships, massages, and programs with potentially dangerous content (e.g. extreme caloric restriction diets) or content by providers with conflicts of interest (e.g. educating and then trying to sell you the necessary supplement) are not supported.
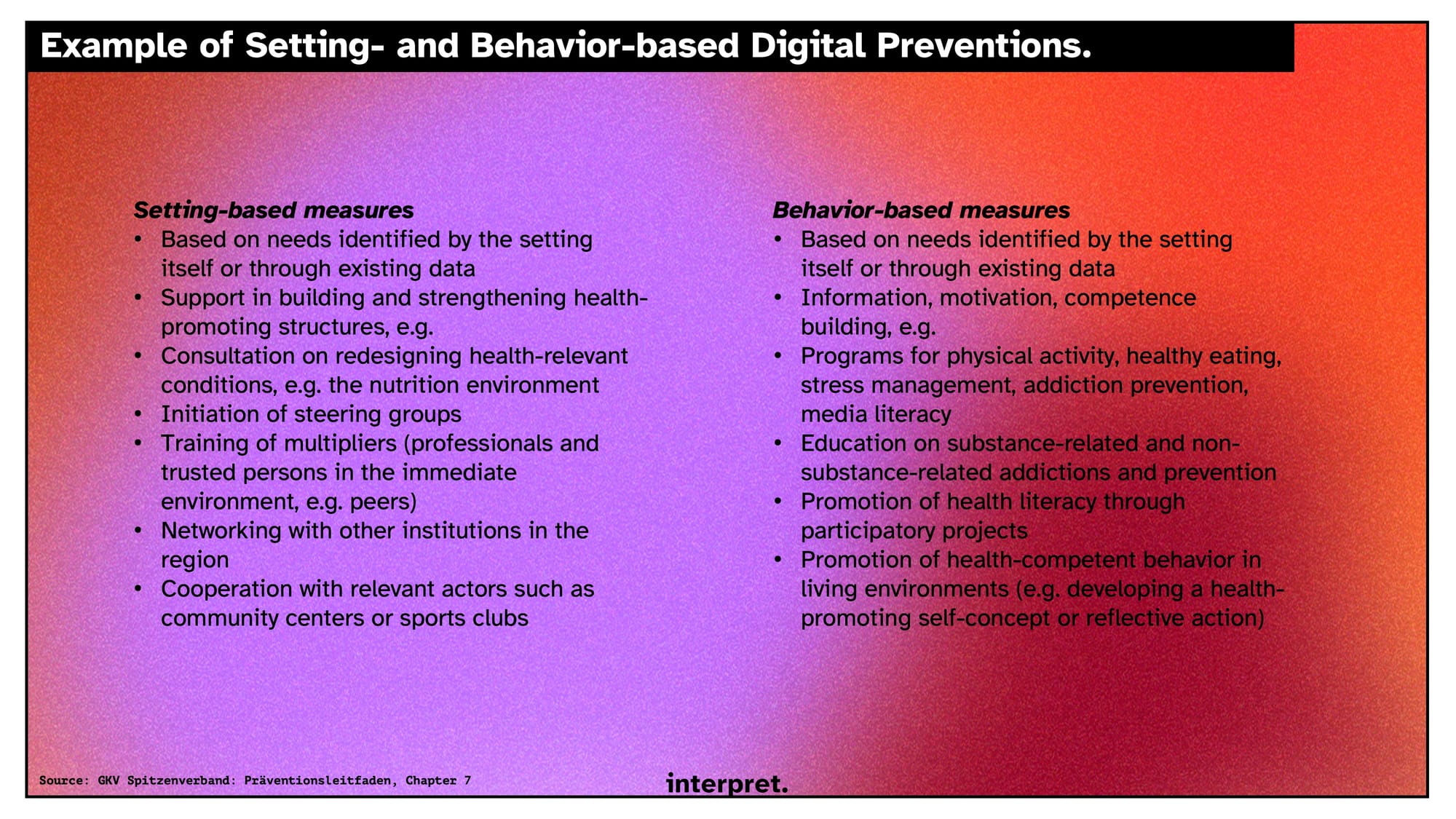
These apps can be either build for individuals as direct interventions or as interventions to change the systems people live in:
Now for the business case
There are obviously plenty of problems to solve for: loneliness, smoking habits, lack of day structure, trouble in friendships, lack of nutrition knowledge, ...
So how do you get a product to market? There is a two-stepped process that distinguishes approved apps from any random app on the internet:
- Concept recognition: A provider first submits a concept that fits a defined prevention field or principle. If its health benefits are not yet proven, it can still be approved for one year if the study design is in place and other criteria are met. Once the study confirms the benefit, recognition is extended to three years. If evidence already exists, the three-year recognition is granted right away.
- Certification of the digital program: With a recognized concept, providers can request certification of their digital prevention or health promotion program. Recognition is limited to three years.
After three years, approval needs to be sought again, through the same process. Applications are centrally vetted by the Zentrale Prüfstelle Prävention as the regulatory body representing all statutory insurers. If approval is successful, you can go and negotiate individual contracts with insurers to get reimbursements for their members.
Comparing to DiGAs, there are a few pros here:
- You don't need a prescription. That saves the visit to the doctor for the patient and turns distribution into a classical marketing problem, as in for a regular wellbeing app. (+ you have the insurer as an additional distribution channel)
- adesso projects that you can earn back the cost of certification within a year (through individual agreements with insurers). They calculate a cost of €400k to get to market, roughly half of what a DiGA would cost.
- Regulation is simpler. Because you are not dealing in therapeutics and measuring the impact of prevention measures is simply more difficult, the standards are significantly looser.
- You can customize the product for each user. There are no rules on the length or structure of the program.
Whilst you might be as exited as I was when hearing about this type of product, I want to leave you with a hefty list of cons to give a more balanced perspective:
- Limited certification timeframes. Needing to reevaluate your product (with the associated bureaucratic and scientific cost) leaves you with a very short product life cycle and a short window of two years to actually make money off of it (assuming you can recuperate all cost in year 1).
- Users need to pay out of pocket to then get reimbursed by their insurers. This makes the sell a lot harder.
- You lack the placebo effect of a doctor prescribing you an app. How likely is it for your user to actually stick to it and see a positive impact from the product?
Worst case I completely ruined it for you, best case you are coming up with ideas as you read this to create the next product or tool in subclinical mental health.
Regardless, have a wonderful week,
Friederich
